Bariatric surgery has transformed the lives of countless individuals battling severe obesity. These surgical procedures not only aid in significant weight loss but also help manage obesity-related health conditions like diabetes and hypertension. But what is a bariatric procedure, and how does it work? Let’s dive into the types, benefits, and insights of bariatric surgical procedures.
A bariatric procedure refers to a range of surgical interventions designed to alter the digestive system for weight reduction. Unlike cosmetic slimming procedures such as liposuction, bariatric surgeries target long-term changes by limiting food intake or reducing nutrient absorption. These weight reduction procedures can improve overall health and quality of life.
Understanding the different types of bariatric procedures is essential to determining the right fit for each individual. Here’s an overview of the most common types:
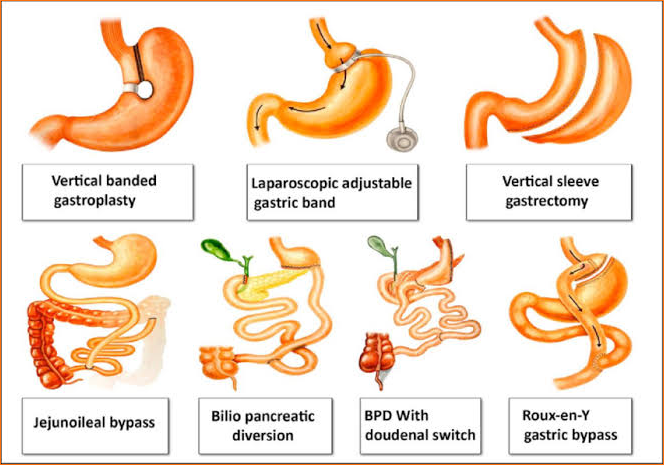
The best procedure depends on factors such as Body Mass Index (BMI), existing health conditions, and lifestyle. The most common bariatric procedures, like the gastric bypass and sleeve gastrectomy, are often recommended for their safety and effectiveness.
Choosing the right procedure isn’t just about the type of surgery—it also depends on key eligibility criteria, safety protocols, and long-term success factors outlined in current clinical guidelines for bariatric surgery.
Post-surgery, patients embark on a new lifestyle journey, commonly referred to as bariatric post-surgery life. This includes:
Studies show that bariatric surgeries can lead to a 50-80% reduction in excess body weight within two years. Gastric bypass remains one of the most commonly performed procedures due to its effectiveness in managing obesity-related conditions.
Bariatric surgery is a life-changing decision that requires thorough research and expert consultation. With different types of bariatric procedures available, finding the right fit is essential for achieving lasting weight loss and improved health. Whether it’s a gastric restrictive procedure or a minimally invasive laparoscopic technique, these surgeries pave the way for a healthier future.
For those considering bariatric surgery in Tampa, FL, consult with specialists at Tampa Weight Loss Institute to explore options and understand the safest bariatric procedure for your needs. Take the first step toward a new life today!
-Disclaimer-
The information provided on this website is for educational and informational purposes only and is not intended as medical advice. Always consult with a qualified healthcare provider regarding any medical concerns, conditions, or treatment options. Individual results may vary. The services described are not intended to diagnose, treat, cure, or prevent any disease. Any medical procedure should be discussed thoroughly with a licensed professional before beginning treatment.

Dr. Amit Taggar is a board-certified, fellowship-trained bariatric surgeon and the founder of Tampa Weight Loss Institute. Recognized globally for his expertise in robotic weight loss surgery, Dr. Taggar specializes in Roux-en-Y gastric bypass, vertical sleeve gastrectomy, duodenal switch, and complex bariatric revisions. He has trained surgeons from around the world and performed live surgical demonstrations at major international conferences.
Committed to empowering patients on their weight loss journey, Dr. Taggar emphasizes a comprehensive approach to long-term success, integrating advanced surgical techniques with personalized aftercare. At Tampa Weight Loss Institute, he leads a team dedicated to transforming lives through compassionate, patient-centered care.