Insurances That Cover Bariatric Revision Surgery
Yes. Many Insurance plans may cover Bariatric Revision Surgery when it is medically necessary. However, the word “cover” is not the same as “approved.” Most patients need Prior Authorization, documentation that matches the plan’s policy criteria, and an In-Network pathway (Surgeon + Facility + Anesthesia).
Most people immediately ask two follow-up questions:
- Which Insurance plans cover Revision Bariatric Surgery?
- What do I need to qualify, and how do I avoid a denial?
Here is all the information you would require:
- Revision Surgery can be covered when there is a medical reason (complications, severe reflux, anatomical issues, or procedure failure).
- Employer plans can vary widely: two patients can both have “BCBS” but different employer rules and exclusions.
- Medicare and Medicaid may cover revisions for eligible patients, but criteria and the process differ (Medicaid varies by State).
- Your out-of-pocket cost still depends on deductibles, coinsurance, copays, and network status.
- Tampa Weight Loss Institute helps verify benefits and build a documentation checklist before submission to reduce delays.
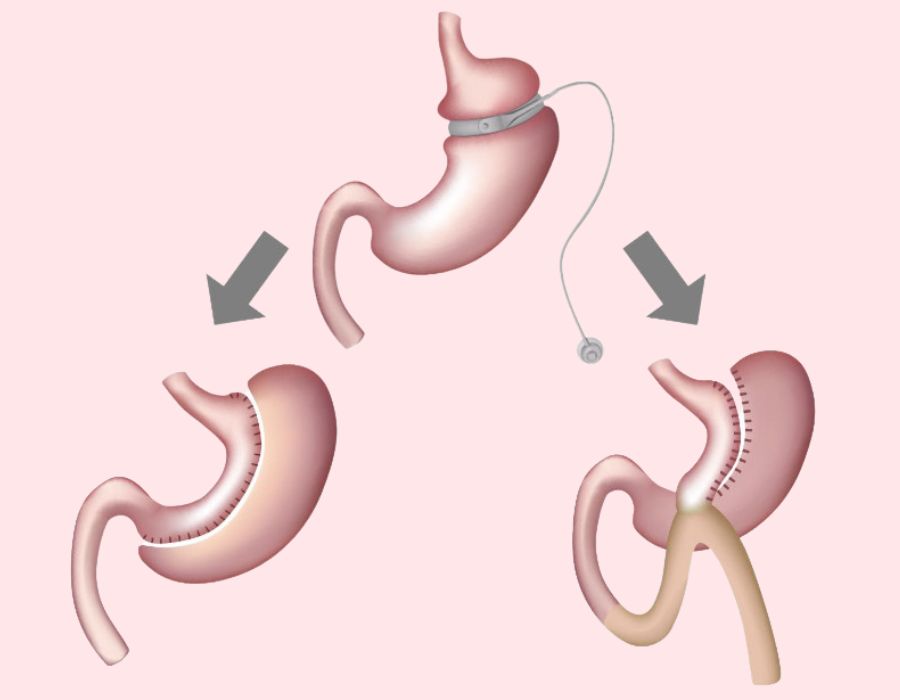
What Counts as Bariatric Revision Surgery
Insurers use specific language, and using the wrong term can slow approvals. Here is the practical difference:
Most plans are more strict about revisions and conversions than primary surgery because they want clear proof of medical necessity, objective findings when relevant, and documentation of conservative treatments attempted.
The Most Common Reasons Insurance Approves Revision Bariatric Surgery
Which Insurances Commonly Cover Bariatric Revision Surgery
For all Insurers, Revision is most likely to be covered when there is Medical Necessity: Complications (especially GERD/Reflux, Stricture, Ulcer, Obstruction), documented Anatomical Failure, or clinically significant failure tied to Health Risk.
However, below are the common Insurance categories and Eligibility Criteria’s for Bariatric Revision Surgery. Availability is plan-specific, and the best next step is always verification.
Blue Cross Blue Shield (BCBS)
Plan you need to have
- An Employer-Sponsored BCBS Plan that includes Bariatric Surgery Benefits (many do, some Employer Plans exclude Bariatric entirely)
- Sometimes an ACA Marketplace BCBS Plan can include Bariatric Benefits, but it depends on the specific Marketplace Product and State rules
- If you have BCBS Federal (FEP), coverage rules are separate from commercial BCBS
Eligibility Criteria
BCBS Plans commonly approve Revision when there is Medical Necessity, such as:
Complications from the original Surgery (severe GERD/Reflux, Stricture, Ulcer, Obstruction, Leak, etc.)
Anatomical Failure or mechanical issue documented by Imaging/Endoscopy
Inadequate Weight Loss or Weight Regain with Medical Risk (not just dissatisfaction)
The chosen Revision is appropriate for the clinical problem (example: severe Reflux after Sleeve often pushes toward a different Revision path than weight regain alone)
UnitedHealthcare
Plan you need to have
- An Employer-Sponsored UnitedHealthcare Plan that includes Bariatric Coverage (Employer Exclusions are common)
- Certain UHC Marketplace Plans may cover Bariatric, depending on the Product and State
- Some members have Employer “Centers of Excellence” pathways (the Benefit exists, but you must use the required route)
Eligibility Criteria
UnitedHealthcare commonly looks for:
Medical Necessity supported by Complications, Anatomy, or documented failure
Complication-Driven Revision (Reflux, Obstruction, Ulcer, Stricture, etc.) tends to be the strongest approval category
Weight Regain / Inadequate Loss must be tied to Health Risk and not explainable purely by non-adherence
Objective findings when relevant (Endoscopy, Imaging, Labs) to show cause and justify Revision type
Aetna
Plan you need to have
- An Employer Aetna Plan that includes Bariatric Surgery Benefits
- Some Aetna Marketplace Plans may cover Bariatric, depending on the Product
- Aetna is very “Policy-driven,” meaning your Plan usually follows a defined Coverage Policy checklist (still Employer-dependent)
Eligibility Criteria
Aetna commonly expects:
- Medical Necessity (Complications, Anatomical Failure, or clinically significant Failure of primary Surgery)
- Documented Complications (severe GERD, Stricture, Ulceration, Obstruction, etc.)
- Failure / Weight Regain with a medically meaningful reason and risk (Comorbidities worsening, high BMI persistence, etc.)
- Evidence that Revision type matches the problem (Reflux-driven vs weight-driven Revision)
Cigna
Plan you need to have
- An Employer Cigna Plan that includes Bariatric Benefits (some Employer Plans exclude Bariatric)
- Some Cigna Marketplace Plans may cover Bariatric depending on the Product and State
- Some Plans route Bariatric through specific Networks or Programs
Eligibility Criteria
Cigna commonly approves Revision when:
- There is clear Medical Necessity (Complications, anatomical/mechanical failure, or clinically significant failure of primary Surgery)
- Complications are documented and persistent despite appropriate treatment
- Inadequate Results are tied to Health Risk (not cosmetic preference)
- Objective evidence supports the need for Revision and supports the selected Procedure
TRICARE
Plan you need to have
- TRICARE Prime or TRICARE Select (Rules differ, Prime usually has stricter Referral/Authorization pathways)
- Eligibility depends on TRICARE status (Active Duty, Retiree, Dependent, etc.)
Eligibility Criteria
TRICARE generally requires:
- Medical Necessity based on complications or failure of primary Surgery
- Clear clinical indication for Revision (complications, anatomy, or failure with medical risk)
- Revision must be appropriate and medically justified (not cosmetic preference)
Medicare
Plan you need to have
- Original Medicare (Part A/Part B) or a Medicare Advantage (Part C) Plan that covers Bariatric procedures
- Coverage is still eligibility-based and can vary by Advantage Plan administration
Eligibility Criteria
Medicare-style criteria are usually built around:
- Medical Necessity (complications or clinically significant failure)
- Eligibility thresholds for Obesity-related disease burden and prior treatment failure (Revision must be justified, not elective)
Medicaid
Plan you need to have
- Florida Medicaid (or your State’s Medicaid) either as Fee-for-Service Medicaid or a Managed Care Medicaid Plan
- Coverage varies by State and Managed Plan, so the “Plan you need” is basically: one that includes Bariatric/Revisional coverage for medical necessity
Eligibility Criteria
Medicaid commonly requires:
- Medical Necessity, especially Complications of prior Surgery
- Objective evidence (when relevant) supporting Revision need
- Revision must be justified as treatment, not cosmetic preference
- State and Managed Plan rules can be more restrictive than commercial Insurance
Employer Benefit Programs (Lantern, Transcarent)
Your Employer must offer Lantern or Transcarent as a Benefit. You must be an eligible covered Member under that Employer’s program.
Eligibility Criteria for Bariatric Revision
Typically:
Program-defined Eligibility Criteria + Medical Necessity
Qualification is often checked upfront, and then you’re guided through an approved pathway (often with very low or $0 out-of-pocket for eligible Members)

SADI Revision: Why It Is Often a Top Option
SADI-S (Single Anastomosis Duodeno-Ileal Bypass with Sleeve) is a metabolic Bariatric procedure that is frequently used as a revision option, especially after Sleeve Gastrectomy. Many surgeons consider it a high-impact revision because it can deliver strong weight loss and metabolic improvements for appropriate candidates.
What Makes SADI a Strong Revision Choice (For the Right Patient)
- It is commonly used as a revision after Sleeve Gastrectomy when additional weight loss or metabolic improvement is needed.
- It may provide excellent outcomes for weight loss and comorbidity control in published clinical studies.
- Compared with some other revision options, studies have reported favorable weight loss outcomes for SADI-S in certain patient groups.
Important: “Best” is personal. The best revision depends on your symptoms (especially reflux), anatomy, prior surgery details, nutrition risk, and what your Insurance policy supports. A consultation and workup determine the safest, most effective option.
Frequently Asked Questions
What if I do not have my original Operative Report?
Will Insurance pay for Excess Skin Removal after Bariatric Surgery?
Is SADI always the best revision?

Next Steps With Tampa Weight Loss Institute
If you are considering Bariatric Revision Surgery, the fastest path is to verify coverage first and then build your documentation around the plan’s criteria.
- Book a consultation to review symptoms, history, and revision options (including SADI when appropriate).
- Request Insurance Verification so we can confirm covered benefits, requirements, and network status.
- Get a documentation checklist tailored to your plan’s revision policy.
Author
-

Dr. Amit Taggar is a board-certified, fellowship-trained bariatric surgeon and the founder of Tampa Weight Loss Institute. Recognized globally for his expertise in robotic weight loss surgery, Dr. Taggar specializes in Roux-en-Y gastric bypass, vertical sleeve gastrectomy, duodenal switch, and complex bariatric revisions. He has trained surgeons from around the world and performed live surgical demonstrations at major international conferences.
Committed to empowering patients on their weight loss journey, Dr. Taggar emphasizes a comprehensive approach to long-term success, integrating advanced surgical techniques with personalized aftercare. At Tampa Weight Loss Institute, he leads a team dedicated to transforming lives through compassionate, patient-centered care.
